FACIAL FRACTURES: UNDERSTANDING YOUR INJURY
WHEN TO SEEK MEDICAL ATTENTION FOR FACIAL FRACTURES?
If you or someone you know is exhibiting any of the symptoms or signs associated with facial fractures detailed below, immediate medical attention is highly recommended. Delaying evaluation and treatment can result in long-term functional deficits and cosmetic deformities.
Understanding the symptoms and physical signs of facial fractures is vital for early diagnosis and effective treatment. We specialize in diagnosing and treating a wide range of facial fractures. Here are the types of fractures we commonly treat:
NASAL FRACTURES
The most common facial fracture, typically resulting from blunt force trauma. The injury may involve the nasal bones and/or cartilage.

IMMEDIATE SYMPTOMS
- Pain: The most immediate and noticeable symptom is localized pain at the site of injury.
- Nosebleeds: A fracture is often accompanied by bleeding from one or both nostrils.
- Swelling: Almost all nasal fractures will show some degree of swelling around the nose and possibly extending into the facial area. Sometimes surgery to treat nasal bone fracture may have to be delayed by a few days till the swelling settles.
- Breathing Difficulties: The swelling or deformity may cause problems breathing through the nose.
- Bruising: Over the course of a few hours or days, you may notice bruising around the nose or eyes.
- Altered Smell: In some instances, your ability to smell might be compromised.
PHYSICAL SIGNS
- Deformity: A visible change in the shape of the nose, either subtle or pronounced, may be evident.
- Crepitus: A grating sound or sensation can be felt when touching the nose, indicative of fractured bone moving against each other.
- Tenderness: Touching the area even lightly may elicit pain, indicating underlying trauma.
- Septal Hematoma: In some cases, a blood clot may form inside the nose, which requires immediate medical attention.
- Deviated Septum: The partition of the nose may buckle, bend, get dislocated or fractured leading to narrowing of the nasal passage and nasal obstruction.
MANDIBULAR (LOWER JAW) FRACTURES
Lower jaw fractures can be categorized into:
- Angle: Occurs near the molars.
- Body: Involves the horizontal portion of the lower jaw.
- Condylar: Near the joint connecting the lower jaw to the skull.
- Symphyseal and Parasmphyseal: Located at the front of the lower jaw, near the chin.
- Multiple sites: Fractures may involve two or more of the above sites.
IMMEDIATE SYMPTOMS
- Pain: Intense, localized pain often at the site of impact.
- Swelling: Prominent swelling at the site of fracture.
- Bruising and Swelling: Visible bruising and/or swelling around the jawline or along the floor of the mouth.
- Open Wound: In cases of compound fractures, there may be an open wound.
- Haemorrhage: Bleeding within the oral cavity may be observed during a clinical examination.
- Ear Pain: Referred pain may extend up to the ear.
- Speech Impediments: Difficulties in articulating certain sounds or words.
- Chewing Difficulties: Experiencing difficulty or discomfort while chewing.
PHYSICAL SIGNS
- Facial Asymmetry: Obvious or subtle changes in the shape of the lower face.
- Jaw Stiffness: A feeling of stiffness or restriction in the jaw.
- Crepitus: Crunching or grinding sounds during jaw movement due to bone fragments.
- Numbness: Loss of sensation along the lower lip or chin due to nerve damage.
- Malocclusion: Improper alignment of the teeth.
- Bite Disruption: An uncomfortable or shifted bite, particularly near the back molars.
ZYGOMATIC (CHEEKBONE) FRACTURES
Cheekbone fractures can disrupt the alignment of the eye and cheek and lead to difficulty in mouth opening. These may require surgical intervention for repair.
PRIMARY SYMPTOMS
- Facial Pain: Sharp or throbbing pain localized to the cheek area, especially when attempting to open the mouth or move the face.
- Swelling: Significant swelling is usually observed over the cheekbone area, extending towards the lower eye rim and side of the face.
- Numbness: You may experience numbness or reduced sensation over the cheek and upper lip due to nerve damage.
SECONDARY SYMPTOMS
- Visual Disturbances: Difficulty moving the eye, double vision, or blurring may occur due to muscle entrapment or swelling.
- Difficulty in Mouth Opening: Discomfort or resistance when opening the mouth is common due to muscle attachment to the zygomatic bone.
- Altered Facial Appearance: There might be an obvious or subtle change in the facial contour, leading to asymmetry.
PHYSICAL SIGNS
- Step-Off Deformity: A physical indent or “step” can be felt along the bone’s edge, often near the lateral eye rim or below the zygoma.
- Bruising: Bruising may develop below the eye or around the cheek, sometimes extending to the neck or chest due to gravity.
- Ecchymosis: ‘Raccoon eyes’ or periorbital ecchymosis may be apparent in severe cases.
- Trismus: Limited mouth opening due to muscle spasm or mechanical blockage by displaced bone fragments.
MAXILLARY (UPPER JAW) FRACTURES

Affecting the upper jaw, these fractures can also impact the alignment of the teeth and the position of the palate. Types include:
- Le Fort I: Horizontal fracture above the upper teeth
- Le Fort II: Pyramidal fracture affecting the nose and upper jaw
- Le Fort III: Transverse fracture that separates the facial skeleton from the cranial base
- Palatal Fractures: These fractures affect the roof of the mouth, involving both the hard palate.
Maxillary fractures, involving the upper jaw, are complex and can significantly affect facial function and appearance. Quick identification and intervention are essential for the best possible outcomes. Here, we provide an in-depth guide to the symptoms and signs of maxillary fractures.
PRIMARY SYMPTOMS
- Pain and Tenderness: Acute pain in the upper jaw, often intensifying when speaking, chewing, or moving the face.
- Swelling: Swelling often extends from the upper jaw to the surrounding facial areas, including the cheeks and lower eye regions.
- Malocclusion: A noticeable change in dental alignment or bite, which may affect eating and speech.
- Bleeding: Blood may be visible in the nose, mouth, or even in the throat, potentially causing difficulty in swallowing.
SECONDARY SYMPTOMS
- Numbness: A loss of sensation in the upper lip, cheek, or palate due to nerve damage.
- Speech Impediments: Problems with articulating sounds, or a “nasal” sounding voice, may occur.
PHYSICAL SIGNS
- Visible Deformity: A distortion in the shape of the upper jaw or midface, which may be subtle or obvious.
- Bruising: Discoloration in the area surrounding the maxilla and possibly extending to the neck and chest.
- Subconjunctival Haemorrhage: Blood visible in the white part of the eyes due to impact force.
- Open Wounds: Lacerations or open wounds may be present, indicating a more severe fracture that has broken the skin.
- Palatal Split: A break or gap may be palpable or visible along the roof of the mouth in some cases.
- Malocclusion: There may be malalignment of teeth between the upper and lower jaw.
ORBITAL (EYE SOCKET) FRACTURES
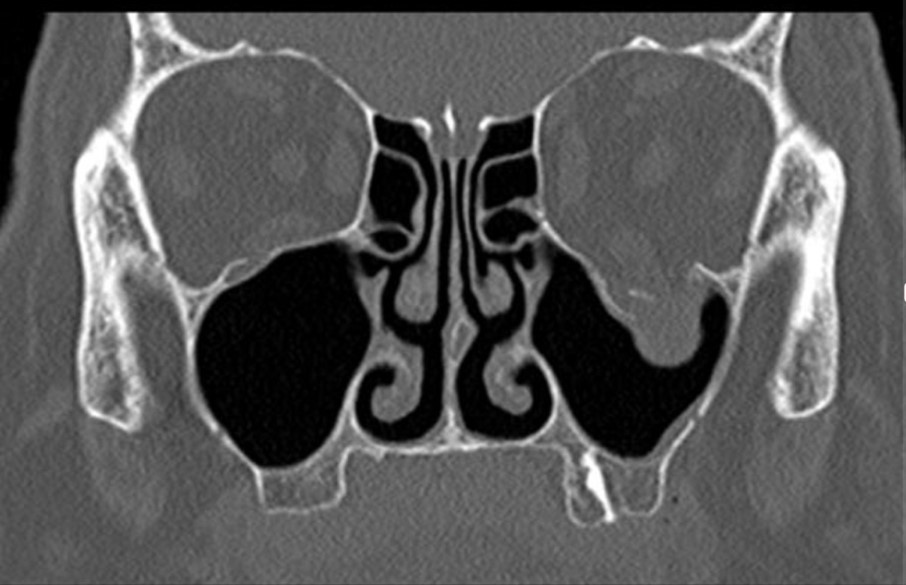
and muscle herniation into the maxillary sinus. fracture.
Damage to the eye socket can result in:
- Blowout: Affects only the floor of the eye socket or the wall between the eye and the nasal sinuses.
- Orbital Rim: Involves the thicker outer rim.
- Complex: Involves multiple bones surrounding the eye like the superior and medial walls along with the floor and the lateral wall.
- Frontal Bone (Forehead and Brow): While rarer, these fractures can extend into the frontal sinuses and even the base of the skull. Frontal bone fractures are relatively rare but can be severe, often resulting from high-impact traumas like motor vehicle accidents or falls from heights. Understanding the symptoms and signs can aid in timely diagnosis and effective treatment.
COMMON SYMPTOMS AND SIGNS
- Nausea or Vomiting: Due to the impact, some clients may experience nausea or vomiting.
- Headache: Severe headaches often occur, particularly in the forehead area. Attention should be sought immediately, especially if there is associated nausea or vomiting or altered consciousness.
- Facial Swelling: Notable swelling may appear above the eyes or across the forehead.
- Visual Disturbances: Blurring or double vision can happen, although less commonly.
- Forehead Deformity: An observable change in the shape or contour (depression) of the forehead may occur.
- Bruising: Bruising often develops, extending to the areas around the eyes.
- Cerebrospinal Fluid Leakage: In severe cases, there may be a leakage of cerebrospinal fluid ( fluid that bathes the brain) from the nose or ears.
- Altered Consciousness: Some clients may experience confusion, dizziness, or even temporary loss of consciousness.
- Periorbital Ecchymosis: Also known as ‘raccoon eyes,’ dark bruising around the eyes may occur.
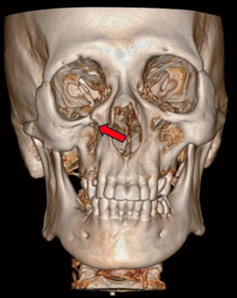
COMPLEX OR COMMINUTED FRACTURES

Whether you have a simple or complex facial fracture, our multidisciplinary team is equipped with the skills and technology to provide you with the best care possible.
OUR GENERAL APPROACH TO MANAGEMENT OF FACIAL FRACTURES
Management of facial fractures is a complex and nuanced process that requires a multi-disciplinary approach, often involving a team of specialists including facial plastic surgeons, oral and maxillofacial surgeons, and sometimes neurosurgeons.
Dr Sandeep and his team are highly skilled in dealing with various types of facial fractures, utilising advanced surgical techniques and contemporary equipment to achieve optimal results.
Below is an overview of the general principles involved in the management of facial fractures at our centre:
ASSESSMENT
The assessment of facial fractures is a critical first step in determining the appropriate course of treatment. The process is multi-faceted and requires a keen eye for detail, along with a comprehensive understanding of facial anatomy and trauma mechanisms. Dr Sandeep and his team have honed their skills in this area, employing a systematic approach that includes the following components:
INITIAL EVALUATION
Triage: Clients are first triaged to assess the severity of their condition and to prioritise their treatment based on urgency.
Primary Survey: An initial assessment is conducted focusing on the client’s airway, breathing, and circulation (ABCs) to identify any life-threatening conditions that may require immediate intervention.
Secondary Survey: This involves a more detailed examination to identify the specific types and locations of fractures.
INITIAL EVALUATION
X-ray: Plain X-rays may provide a preliminary assessment but are often insufficient for detailed planning.
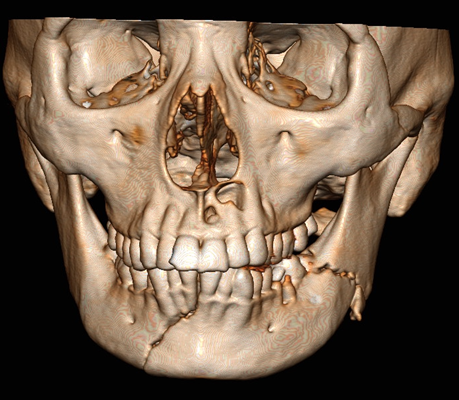
Computed Tomography (CT) Scan: This is the gold standard for assessing facial fractures. It offers detailed cross-sectional images and can even be rendered into 3D images for better visualization.
Magnetic Resonance Imaging (MRI): Rarely used for bone fractures but may be employed for associated soft tissue injuries.
CLINICAL EXAMINATION
Visual Inspection: The team inspects for signs such as facial asymmetry, deformity, bruising, or lacerations that might indicate a fracture.
Palpation: Manual examination is performed to assess for tenderness, crepitus, or step-off deformities in the bone structure.
Functional Tests: The client’s ability to open and close the mouth, eye movements, and sensory function are tested.
Dental Occlusion: An assessment of how the teeth meet when the jaw is closed can provide clues to underlying fractures.
IMAGING STUDIES
X-ray: Plain X-rays may provide a preliminary assessment but are often insufficient for detailed planning.
Computed Tomography (CT) Scan: This is the gold standard for assessing facial fractures. It offers detailed cross-sectional images and can even be rendered into 3D images for better visualization.
Magnetic Resonance Imaging (MRI): Rarely used for bone fractures but may be employed for associated soft tissue injuries.
SPECIALIST CONSULTATIONS
In complex cases, Dr Sandeep may consult with other specialists such as:
Ophthalmologists: For assessment of vision and injury to the globe for fractures that might affect the eye or orbital region.
Neurosurgeons: For fractures that extend into the cranial cavity or involve the base of the skull.
Oral and Maxillofacial Surgeons: For fractures involving dental structures.
DOCUMENTATION
Medical Records: Detailed documentation is maintained, including the client’s medical history, clinical findings, and imaging studies.
Photographic Records: Preoperative photographs may be taken for the medical record and for planning surgical interventions.
CLASSIFICATION
Facial fractures are classified based on the area affected—such as the mandible, maxilla, or zygoma—to determine the best treatment approach.
PLANNING
Through this rigorous and systematic assessment process, Dr Sandeep and his team are able to accurately diagnose the type and extent of facial fractures. This allows them to formulate a tailored treatment plan, aimed at restoring both function and aesthetics to the highest possible standard.
SURGICAL INTERVENTION
OPEN REDUCTION AND INTERNAL FIXATION (ORIF)
Open Reduction and Internal Fixation (ORIF) is a surgical technique commonly used in the treatment of complex facial fractures. This is often the treatment of choice for complex fractures. Dr Sandeep uses miniature screws and plates to align and fix the fractured bones.
PREOPERATIVE PREPARATION
Client Counselling: Detailed discussions are held with the client to explain the procedure, risks, and expected outcomes.
Anaesthetic Evaluation: Clients are assessed for their suitability for anaesthesia, which can be either general or local depending on the complexity of the fracture.
Surgical Planning: High-resolution imaging studies, often 3D-rendered, are reviewed to plan the surgical approach and fixation methods.
SURGICAL PROCEDURE
Anaesthesia: After induction of anaesthesia, the client is positioned to allow optimal access to the fracture site.
Incision: The initial incision is carefully planned to ensure minimal scarring. Common approaches include intraoral incisions for maxillary and mandibular fractures, and subciliary or transconjunctival incisions for orbital fractures.
Exposure and Identification: The fractured bone segments are exposed using surgical retractors, and the extent of the fracture is identified.
Reduction: The fractured bones are manually aligned back into their anatomical position.
Temporary Fixation: Temporary fixation may be applied using surgical clamps or wires to hold the bones in place.
Internal Fixation: Titanium plates, screws, or mesh are used to secure the bones. The choice of hardware depends on the fracture type and location.
Closure: After confirming the alignment using intraoperative imaging or manual inspection, the incision is closed using sutures that are either absorbable or will be removed at a later stage.
POSTOPERATIVE MANAGEMENT
Immediate Monitoring: Clients are monitored in the postoperative recovery area for vital signs, pain, and any complications like bleeding.
Pain Management: Analgesics are administered to manage postoperative pain.
Antibiotics: Prophylactic antibiotics may be administered to prevent infection.
Dietary Adjustment: A soft or liquid diet may be advised initially to avoid stress on the healing fractures.
Physical Therapy: Clients may be referred for physiotherapy to improve facial function and range of motion.
Follow-up: Regular follow-up appointments are scheduled for wound inspection, removal of sutures, and imaging studies to confirm healing.
SPECIAL CONSIDERATIONS
Aesthetic Concerns: Dr Sandeep takes extra precautions to ensure that any scarring is minimal and as inconspicuous as possible. Touch up procedures may be needed in certain clients if there is residual aesthetic deformity after primary surgery, especially for very complex fractures.
By following this comprehensive approach to ORIF of facial fractures, Dr Sandeep and his team are able to achieve excellent outcomes, restoring both function and aesthetics to the affected facial regions.
CLOSED REDUCTION
Closed reduction is another surgical technique employed in the treatment of facial fractures, particularly for less complex or minimally displaced fractures. For simpler fractures, a closed reduction might be sufficient, which involves manually aligning the fractured bones without the need for incision or internal fixation.
Below is a detailed account of how closed reduction is performed for facial fractures:
PREOPERATIVE CONSIDERATIONS
Client Assessment: A thorough evaluation, including imaging studies, is conducted to determine the suitability of closed reduction.
Informed Consent: The risks, benefits, and limitations of closed reduction are discussed with the client.
Anaesthesia Assessment: A review is conducted to decide on the type of anaesthesia, which could be local, regional, or general.
PROCEDURE STEPS
Anaesthetic Administration: Anaesthesia is administered to numb the area or sedate the client, depending on the type chosen.
Manual Alignment: Dr Sandeep or a member of his team manually manipulates the fractured bones to bring them back to their anatomical position. This may involve the use of instruments like elevators or forceps.
Temporary Fixation: After achieving satisfactory alignment, temporary fixation methods such as intermaxillary fixation (IMF) with wires or elastics may be used to maintain the position.
Radiological Verification: Imaging studies like X-rays or CT scans may be taken intraoperatively to confirm the success of the reduction.
Additional Support: Sometimes, external devices like splints or bandages may be applied to provide additional support during the healing process.
POSTOPERATIVE MANAGEMENT
Immediate Monitoring: Vital signs and pain levels are closely monitored in the immediate postoperative period.
Pain Relief: Analgesics are administered as needed for pain control.
Soft Diet: A soft or liquid diet may be recommended to avoid putting stress on the healing bones.
Follow-up Appointments: Regular follow-up visits are scheduled for clinical and radiological assessment of the healing process.
Removal of Temporary Fixation: If intermaxillary fixation or other temporary methods were used, these are usually removed at a later stage once sufficient healing has occurred.
Rehabilitation: Physiotherapy may be recommended for optimal functional recovery.
ADVANTAGES AND LIMITATIONS
Less Invasive: Closed reduction is less invasive than ORIF, resulting in fewer complications like infection or scarring.
Faster Recovery: The recovery period is generally quicker as there are no surgical incisions to heal.
Limitations: Closed reduction is generally suitable for less complex fractures and may not provide as stable a fixation as ORIF.
Aesthetic Concerns: While closed reduction is less invasive, it may sometimes result in less optimal aesthetic outcomes compared to ORIF, especially if the fractures are complex.
By employing closed reduction when suitable, Dr Sandeep and his team offer clients a less invasive option for the treatment of facial fractures, with the aim of restoring both function and appearance with minimal surgical intervention.
OBSERVATION
Observation as a treatment strategy is generally reserved for certain types of facial fractures that are minimally displaced, stable, and do not pose a risk to surrounding structures such as the eyes, airways, or important nerves. Dr Sandeep and his team consider observation as a viable option when surgical intervention is not deemed necessary for functional or aesthetic reasons. Here is a comprehensive overview of when and how observation is used as a treatment modality for facial fractures:
CRITERIA FOR OBSERVATION
Minimal Displacement: The fractured bones should be close to their anatomical position.
Stable Fractures: There should be no risk of the fracture becoming displaced under normal conditions.
No Functional Impairment: The fracture should not impede essential functions like vision, breathing, or eating.
No Cosmetic Concerns: The fracture should not result in significant aesthetic deformities.
MONITORING AND FOLLOW-UP
Initial Evaluation: A thorough initial assessment is conducted to rule out any factors that may necessitate surgical intervention.
Regular Checks: Clients are asked to come in for regular follow-up appointments for clinical and radiological assessment.
Symptom Management: Pain, swelling, or other symptoms are managed conservatively with medications.
Dietary Advice: A soft diet may be recommended initially to avoid putting stress on the healing fracture.
Rehabilitation: Physiotherapy may be recommended for optimal functional recovery.
ADVANTAGES OF OBSERVATION
Non-Invasive: No surgical intervention means fewer risks related to anaesthesia, infection, or scarring.
Cost-Effective: Observation eliminates the costs associated with surgery and hospitalisation.
Quick Recovery: Clients can usually resume normal activities sooner, as there is no postoperative healing time to consider.
LIMITATIONS AND RISKS
Potential for Non-Union: The fractured bones may not heal properly, requiring later intervention.
Functional Limitations: Some fractures may result in functional impairments if not surgically corrected.
Aesthetic Risks: There is a possibility that the fracture heals in a way that causes a cosmetic deformity.
Regular Monitoring: Close follow-up is essential to ensure that the fracture is healing as expected and to detect any complications early.
SPECIAL CONSIDERATIONS
Client Compliance: Observation as a treatment strategy requires the client to follow medical advice closely and to attend all follow-up appointments.
Lifestyle Modifications: Clients may be advised to refrain from activities that could risk further injury.
Psychological Aspect: Some clients may require emotional or psychological support, particularly if the facial fracture has caused stress or anxiety.
By opting for observation as a treatment strategy, Dr Sandeep and his team aim to offer a less invasive yet effective way to manage selected facial fractures. This approach is always backed by a thorough assessment and close monitoring to ensure that it meets the client’s functional and aesthetic needs. This may be the preferred option if the fracture in undisplaced and stable and is not leading to any functional deficit.
ENHANCE YOUR WELL-BEING: SPECIALIZED FACIAL FRACTURE MANAGEMENT WITH DR SANDEEP
Has a facial injury impacted your life? Our Facial Fracture Management Service specializes in the careful assessment and treatment of facial injuries, aiming to restore both function and aesthetics. With our precise and sensitive approach, we prioritize your health and peace of mind.
Recover your facial structure and regain confidence. Begin your recovery with expert care today. Schedule a tailored facial fracture management consultation with Dr Sandeep.


