Hearing loss is a common condition, but when it occurs suddenly, it can be alarming and distressing. Sudden Hearing Loss (SHL) is typically defined as a rapid onset of hearing impairment over a period of 72 hours or less. It is crucial to seek immediate medical attention as early intervention improves the chances of recovery.
Causes of Sudden Hearing Loss
Sudden hearing loss can be classified into conductive and sensorineural types:
1. Conductive Hearing Loss
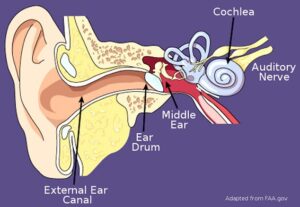
Conductive hearing loss occurs when sound waves cannot reach the inner ear due to obstructions or abnormalities in the outer or middle ear. Causes include:
- Earwax impaction: Excessive earwax can block the ear canal, preventing sound from reaching the eardrum. This is a common and reversible cause of hearing loss that can be treated with ear irrigation or microsuction.

- Acute otitis media (middle ear infection): Infections in the middle ear cause fluid buildup behind the eardrum, leading to temporary hearing loss. If untreated, chronic infections can result in persistent conductive hearing loss

- Otosclerosis: A hereditary condition where abnormal bone growth in the middle ear interferes with sound transmission. It typically affects the stapes bone and can lead to progressive hearing loss, often requiring surgical treatment.

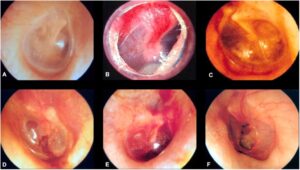
- Barotrauma: Sudden changes in pressure (e.g., during air travel or diving) can damage the eardrum or middle ear structures, causing temporary or permanent hearing impairment. In the following clinical photographs B to F show various presentations of barotrauma to the ear. A is normal ear drum.
- Tympanic membrane perforation (e.g., due to earbud use or trauma): Inserting objects like cotton swabs or earbuds too deeply into the ear canal can rupture the eardrum, resulting in sudden hearing loss. In most cases, the perforation heals spontaneously, but larger defects may require surgical repair.

- Cholesteatoma: An abnormal skin growth in the middle ear that can erode bones and lead to conductive hearing loss. It often requires surgical removal to prevent complications.
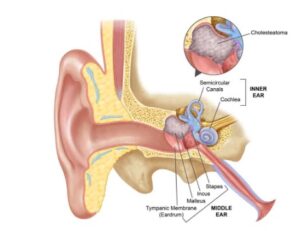
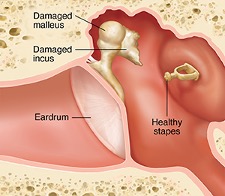
- Ossicular chain disruption due to trauma: Direct trauma to the head or ear can dislocate the ossicles (tiny bones in the middle ear), leading to significant hearing loss. Surgical intervention may be needed.
2. Sensorineural Hearing Loss (SNHL)
Sensorineural hearing loss results from damage to the inner ear (cochlea) or auditory nerve pathways.
Causes include:
- Idiopathic Sudden Sensorineural Hearing Loss (ISSNHL): A sudden loss of hearing with no identifiable cause, often presumed to be viral or immune-mediated. Prompt treatment with corticosteroids is crucial for recovery.
- Viral infections (e.g., herpes simplex virus, cytomegalovirus): Certain viral infections can damage the cochlear nerve or hair cells, leading to permanent hearing impairment. Reactivation of latent viruses may also contribute to sudden hearing loss.
- Bacterial infections (e.g., syphilis, Lyme disease, meningitis): Bacterial infections affecting the inner ear or nervous system can lead to irreversible sensorineural hearing loss. Early antibiotic treatment is essential.
- Ototoxic drugs (e.g., aminoglycosides, cisplatin, loop diuretics): Some medications can damage the hair cells in the cochlea, causing progressive or sudden hearing loss. Monitoring drug levels and using alternative medications when possible is recommended.


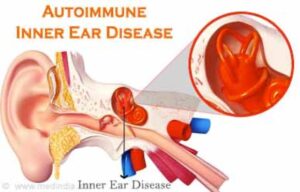
- Autoimmune inner ear disease: An immune-mediated attack on the inner ear structures can cause fluctuating or progressive sensorineural hearing loss, often requiring immunosuppressive therapy.
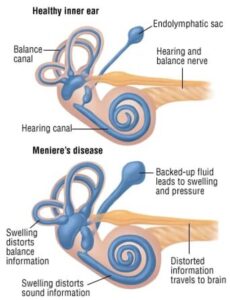
- Meniere’s disease: Characterized by episodic vertigo, fluctuating hearing loss, tinnitus, and aural fullness, this disorder is associated with excess fluid in the inner ear.
- Acoustic neuroma (vestibular schwannoma): A benign tumour on the vestibulocochlear nerve that can cause unilateral hearing loss, tinnitus, and balance issues. MRI is essential for diagnosis.

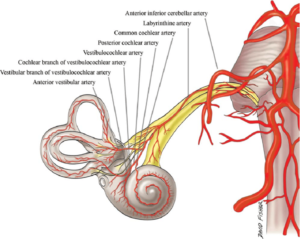
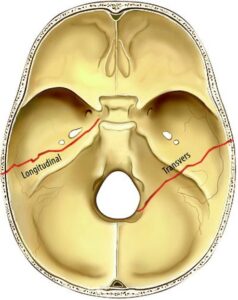
- Vascular events (e.g., microvascular ischemia, stroke): Reduced blood supply to the cochlea or auditory nerve can result in sudden hearing loss. Cardiovascular risk factors should be assessed.
- Trauma (e.g., temporal bone fractures, barotrauma): Blunt force injuries or rapid pressure changes can damage inner ear structures, leading to permanent hearing loss.
Consultation and Diagnosis
Initial Assessment
- Detailed history (onset, associated symptoms like vertigo, tinnitus, or aural fullness)
- Physical examination
- Otoscopy and ear microscopy: To assess the ear canal, tympanic membrane integrity, and signs of infection or trauma.
- Ear endoscopy: Provides a detailed view of the external and middle ear structures.

- Tuning fork tests (Rinne and Weber tests): Helps differentiate conductive from sensorineural hearing loss.
- Nasal endoscopy: Evaluates Eustachian tube function and detects nasopharyngeal tumours affecting the auditory pathway.

Audiological Investigations
- Pure Tone Audiometry (PTA): Confirms sensorineural vs. conductive hearing loss.

- Speech Audiometry: Assesses speech recognition and comprehension at different volume levels, helping to differentiate sensorineural from conductive hearing loss.
- Tympanometry: Measures middle ear pressure and eardrum mobility, aiding in the diagnosis of conditions such as otitis media, Eustachian tube dysfunction, or ossicular chain abnormalities.

- Otoacoustic Emissions (OAE): Assesses cochlear hair cell function.
- Auditory Brainstem Response (ABR): Rules out retrocochlear pathology (e.g., acoustic neuroma).
Radiological and Laboratory Investigations
- MRI with contrast (gold standard): Detects acoustic neuroma, demyelinating disease, or vascular abnormalities

- CT scan (if trauma or cholesteatoma is suspected).
- Blood tests:
- Complete Blood Count (CBC): Checks for infections or haematological abnormalities.
- Erythrocyte Sedimentation Rate (ESR) & C-reactive Protein (CRP): Evaluates for inflammatory or autoimmune conditions.
- Autoimmune Panel (ANA, RF, antiphospholipid antibodies, ANCA): Assesses for autoimmune inner ear disease.
- Viral Serology (HSV, CMV, HIV, EBV, VZV, syphilis serology): Screens for infectious causes.
- Thrombophilia Screen (Protein C, Protein S, Antithrombin III, Factor V Leiden mutation, Homocysteine levels): Identifies vascular aetiologies.
- Metabolic Panel (Glucose, Lipid profile, Thyroid function tests, Vitamin B12): Rules out metabolic contributions.
Treatment of Sudden sensorineural Hearing Loss (SSNHL)
- Systemic Corticosteroids (First-line Treatment)
- Prednisolone 1 mg/kg/day (max 60 mg/day) for 7–14 days with a tapering dose.
- Studies support corticosteroids as the primary therapy for ISSNHL.
- Intratympanic Steroid Injection (ITSI)

- Indications: Poor response to oral steroids, contraindications to systemic corticosteroids, or as an adjunct therapy with oral steroids.
- Procedure: Direct delivery of dexamethasone (4-10 mg/mL) into the middle ear, absorbed through the round window.
- Evidence: ITSI has been shown to be effective as a salvage therapy with better hearing recovery.
- Hyperbaric Oxygen Therapy (HBOT)

- Mechanism: Increases oxygen delivery to the cochlea, promoting hair cell recovery.
- Protocol: 10–20 sessions of 90–120 minutes at 2.0–2.5 ATA pressure.
- Evidence: HBOT combined with steroids leads to better hearing recovery outcomes.
- Other Treatments
- Antiviral therapy: Use is controversial and not routinely recommended unless a viral aetiology is strongly suspected.
- Vasodilators and antithrombotics: Limited role; some studies explored pentoxifylline, heparin, or prostaglandins, but efficacy is unproven.
Prognosis and Follow-Up
- Recovery varies; 50% of patients improve spontaneously.
- Better prognosis if treatment is started within 2 weeks.
- Poorer outcomes with severe hearing loss, older age, and comorbidities.
- Regular audiometry follow-up is essential.
Precautions to Protect Residual Hearing After Sudden Sensorineural Hearing Loss (SSNHL)
If you have experienced sudden sensorineural hearing loss (SSNHL) and have already been seen by an ENT specialist with treatment initiated, the next critical step is to protect your residual hearing and prevent further deterioration. Here are the key precautions to follow:
1. Protect Your Ears from Loud Noises
Exposure to loud sounds can further damage the delicate hair cells in the inner ear, worsening hearing loss.
- Avoid noisy environments (e.g., concerts, nightclubs, heavy traffic, construction sites).
- Use earplugs or noise-canceling headphones in loud settings.
- Keep the volume at safe levels when using headphones or watching TV. Follow the 60/60 rule – keep volume at 60% or lower and limit use to 60 minutes at a time.
- Be cautious with sudden loud sounds (e.g., fireworks, gunfire, explosions) and avoid unnecessary exposure.
2. Avoid Ototoxic Medications
Some medications can be toxic to the inner ear (ototoxic) and may cause further hearing damage.
- Always inform your doctor about your hearing condition before starting new medications.
- Common ototoxic drugs to avoid unless necessary:
- Aminoglycoside antibiotics (e.g., gentamicin, streptomycin)
- High-dose aspirin and NSAIDs (e.g., ibuprofen, naproxen)
- Loop diuretics (e.g., furosemide, bumetanide)
- Certain chemotherapy drugs (e.g., cisplatin, carboplatin)
3. Maintain Good Ear Health
- Avoid inserting objects (cotton buds, ear candles) into your ears.
- Keep your ears dry and clean to prevent infections, which can worsen hearing loss.
- If you have a history of ear infections, seek prompt treatment to avoid complications.
4. Minimize Exposure to Sudden Pressure Changes
Barotrauma (pressure-induced ear damage) can further compromise residual hearing.
- Avoid air travel for a few weeks, if possible, especially if you have ear fullness or pressure issues.
- When flying, use earplugs, swallow frequently, or perform the Valsalva manoeuvre to equalize pressure.
- Avoid scuba diving, as rapid pressure changes can be harmful.
- Be cautious in high-altitude environments (mountains, elevators in tall buildings).
5. Manage Stress and Sleep Well
- Stress and fatigue can worsen tinnitus and impact hearing function.
- Practice stress-reducing techniques such as meditation, yoga, or breathing exercises.
- Ensure adequate sleep, as poor sleep quality may affect hearing recovery.
6. Monitor and Manage Other Health Conditions
Certain medical conditions can negatively impact hearing over time.
- Control high blood pressure and diabetes, as poor circulation can damage inner ear structures.
- If you have autoimmune conditions (e.g., lupus, rheumatoid arthritis), follow your doctor’s advice closely.
- Maintain cardiovascular health, as good blood flow is essential for inner ear function.
7. Follow a Hearing-Friendly Diet
- Reduce salt intake, especially if you have Meniere’s disease or fluid retention issues in the ear.
- Eat a balanced diet rich in antioxidants and vitamins (e.g., vitamin C, magnesium, and zinc) to support nerve health.
- Stay hydrated, as dehydration can affect the inner ear’s fluid balance.
8. Continue Hearing Monitoring and Follow-Up Care
- Attend regular follow-up appointments with your ENT specialist or audiologist.
- Repeat hearing tests as recommended to track any changes.
- If hearing loss persists, consider hearing rehabilitation options such as hearing aids, cochlear implants, or assistive listening devices.
9. Be Cautious with Physical Activity
- Avoid contact sports or activities with a high risk of head trauma, as injuries can worsen hearing issues.
- If you experience dizziness or imbalance, take precautions to prevent falls.
10. Use Assistive Listening Devices if Needed
- If you have persistent hearing difficulties, consider hearing aids or assistive devices to improve communication.
- Use captioning services for TV or phone conversations.
- Inform colleagues and family members about your hearing needs so they can accommodate you in conversations.
Final Thoughts
After SSNHL, protecting your residual hearing is critical to maintaining the best possible quality of life. By avoiding loud noises, managing your health, staying hydrated, avoiding ototoxic medications, and following up with your ENT specialist, you can prevent further hearing deterioration.
Sudden Sensorineural Hearing Loss (SSNHL) – Act Fast, consult with Dr. Sandeep for treatment in singapore!
If you or someone you know experiences sudden hearing loss, don’t wait! Sudden Sensorineural Hearing Loss (SSNHL) is a medical emergency that requires immediate attention. Early diagnosis and treatment can significantly improve your chances of recovery.
Dr. Sandeep, an expert in ENT – Head & Neck Surgery and Facial Plastic Surgery, provides urgent evaluation and advanced treatment for SSNHL. With a personalized approach and the latest medical interventions, he ensures you receive the best care possible.
🔹 Recognize the signs – Sudden hearing loss, ear fullness, dizziness, or ringing in the ear.
🔹 Seek help immediately – Delaying treatment can lead to permanent hearing damage.
🔹 Expert care you can trust – Comprehensive ENT expertise with a focus on functional and long-term hearing health.
📞 Book an urgent consultation now! Time is critical—let’s work together to restore your hearing.


